Causes & Symptoms
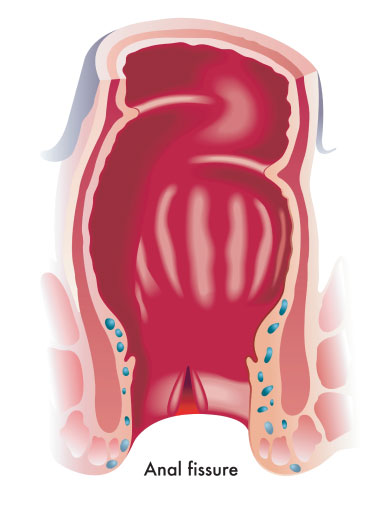
Anal Fissure
How Does It Form?
Characterised as a split (tear) in the lining of the anus, an anal fissure commonly arises from excessive stretching of the anal lining, which often occurs from the passage of hard, dry stools in cases of severe constipation.
The stools cause friction against the sensitive anal canal during bowel movements, resulting in the tearing of the delicate anal lining. This triggers muscle spasms within the internal anal sphincter, making bowel movements even more challenging and requiring added force. As a result, deeper and repeated tearing occurs, with the fissure becoming chronic.
Who Is At Risk?
Apart from constipation or persistent diarrhoea, those undergoing pregnancy and childbirth, or with certain medical conditions (such as inflammatory bowel disease) are known to be at a higher risk of developing anal fissures.
Often accompanied by bleeding, an anal fissure can induce significant pain. Seek prompt medical attention with a colorectal specialist to relieve your pain as quickly as possible.
Schedule A Consultation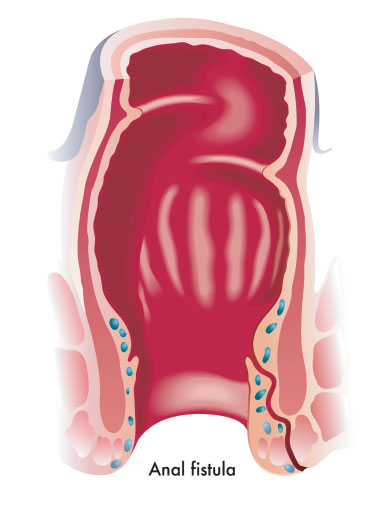
Anal Fistula
What Are The Causes?
Beginning with an infection in an anal gland that results in the buildup of pus (abscess) in nearby tissues, an anal fistula occurs when the abscess bursts and pus drains away, creating a narrow tunnel which gradually develops into an anal fistula after repeated infections.
What Increases The Risk?
While an anal fistula usually forms after an anal abscess, it can also occur as a result of conditions that affect the lower digestive tract or anal area, which include Crohn’s disease, diverticulitis, and chronic diarrhoea.
An anal fistula typically does not heal on its own without surgical intervention. If left untreated, symptoms can persist and recur, and risk infection and damage to the anal sphincter muscles.
To schedule treatment with Singapore experienced colorectal surgeon, Dr Ng Kheng Hong, call +65 6475 5512 or WhatsApp +65 8228 5578.
Anal Fissure or Anal Fistula:
Which Do I Have?
While anal fissure and anal fistula share similar symptoms of bleeding and pain in the anal region, the degree of pain and other symptoms associated with the two conditions vary considerably.
Anal Fissure
- Often results in an intense, burning pain, irritation around the anus and blood in stools during bowel movements.
- Does not have an external opening or extend into a tract.
Anal Fistula
- Characterised by soreness and the presence of foul-smelling discharge from the affected opening, in addition to persistent, throbbing pain.
- Severe cases may also exhibit symptoms such as fever and chills.
The treatment of a fissure or fistula depends on its type, location, severity and size; with the main goal to promote healing, and reduce spasm and pain. To obtain an accurate diagnosis and appropriate treatment plan for your rectal pain, see a colorectal specialist.